At the moment, patients seeking a biological repair strategy would have two places to turn to for tissue replacements: using tissue from another part of their body, or waiting for a donor.
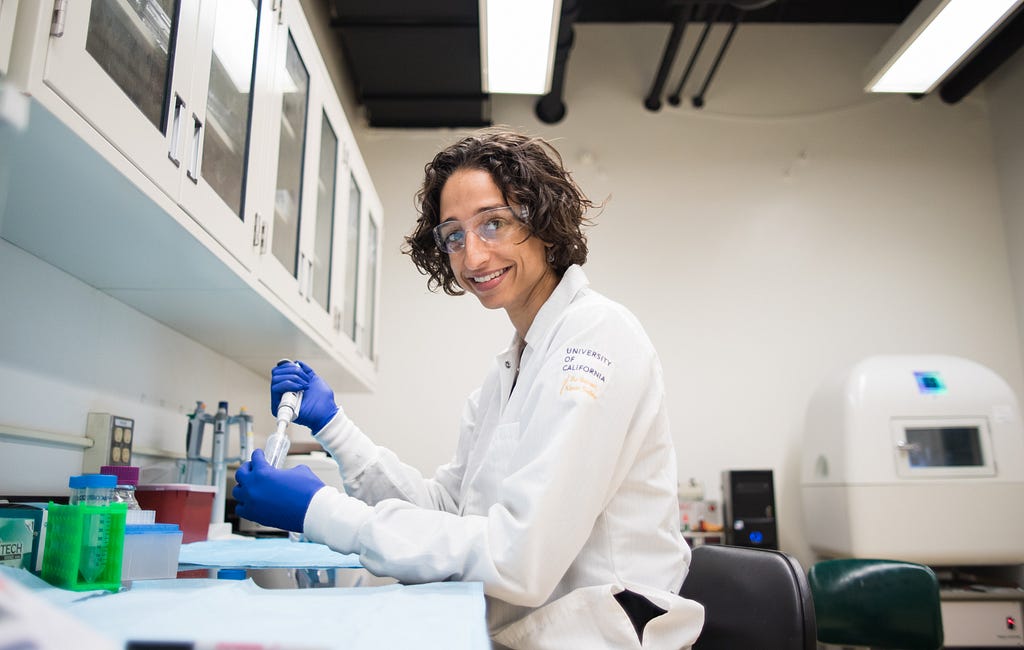
“A surgeon might take tissue from somewhere else in the body, or they can take tissue from a cadaver to repair damaged cartilage.” says O’Connell. “However, a limitation with biological repair strategies is with the amount of tissue available. If we are able to engineer tissue in the laboratory, then you could decrease the tissue shortage problem.” Making tissues that acts just like healthy native tissue in the body is a delicate and lengthy process. Currently, creating tissue in the lab takes about 6 to 8 weeks. In that timeframe, scientists use a 3D printer to create a hydrogel scaffold, which will be the base for creating complex tissue. Stem cells are added to this scaffold and carefully monitored until they have fully dispersed throughout. “It’s all about timing.” says Professor O’Connell. “You don’t just want the cells hanging out in air for long periods of time while you’re creating the engineered tissue.” She explains, “They need constant nutrition. Cells exposed to air will dry up or ‘starve’ if they are not in an aqueous condition for too long.” This becomes a problem when bioprinting larger tissues with longer print times, because cells would not be able to survive through the long bioprinting process. By printing the scaffold first and adding the cells after the fact, Professor O’Connell can prevent cell death, even in large structures.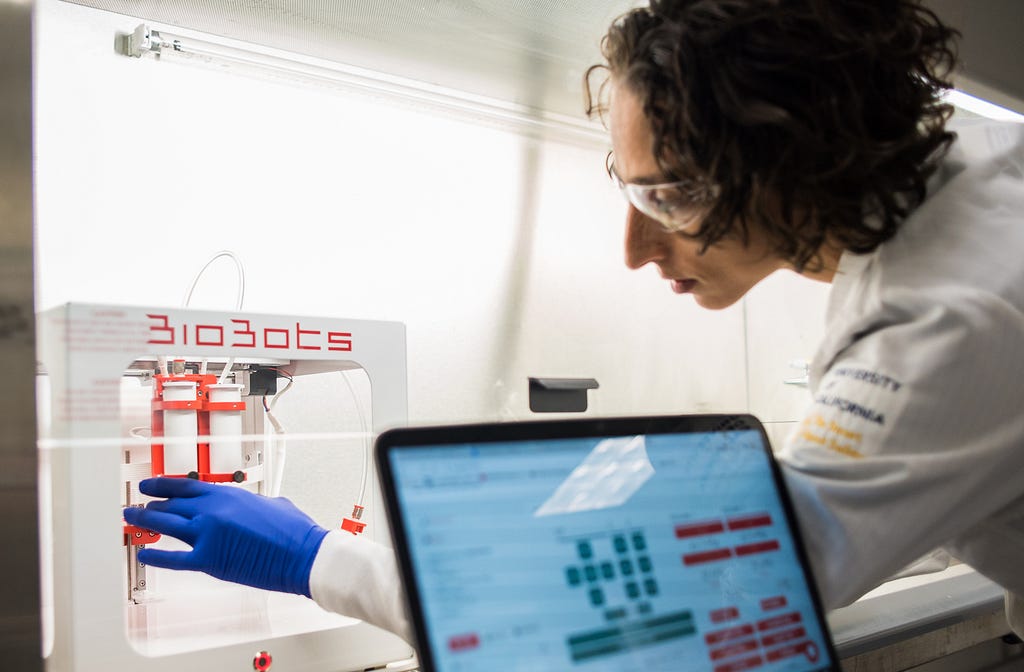
Bio-replacement strategies would delay or eliminate the need for a total joint replacement with metal and plastic components.
“Total joint replacement surgery is being performed in younger and younger patients. 45, 50 years old,” explains Professor O’Connell. “So if you think about the fact that they last 15 years or so and patients are living longer these days, then they have to get a second revision surgery, and sometimes even a third. If there was a biological option for younger patients, even if it doesn’t last forever, at least it would delay getting the total knee replacement, the metal-plastic version.”
Though there are a lot of exciting possibilities in the future of 3D printed tissue there is still a long road ahead before this technology is approved for patients.
Currently, Professor O’Connell and her lab are focusing on studying how well lab-created tissues compare to healthy native tissues. The next steps will be to test lab-created tissues in large mammals and, one day, humans. Professor O’Connell is continuing her research with the knowledge that her work will pay off in tangible benefits for patients.3D Printers & The Future of Tissue Engineering was originally published in Berkeley Master of Engineering on Medium, where people are continuing the conversation by highlighting and responding to this story.